Liver cancers, especially when early in their genesis, are usually asymptomatic. Often they are detected when an ultrasound scan, a CT scan or MRI are performed for other reasons, or when a patient has underlying liver disease (cirrhosis of any cause increases one’s risk of developing liver cancer). So when an imaging study reveals a suspicious lesion in the liver and it has certain defining characteristics, the current medical practice is to proceed with treatment without obtaining a biopsy of the tumor unless there is some doubt as to whether it is truly cancerous or not. The main reason for not biopsying is that we do not what to do with the information.
The Pathologist can tell us that the biopsy shows a well differentiated (good) or poorly differentiated (bad) tumor, but this information does not direct our therapeutic approach. Currently, a liver cancer is a liver cancer and they are all treated similarly. Our only metrics of an individual tumor’s biology are how big is it, how many are there, and how fast is it growing. (Spread outside of the liver, or metastatic disease, and tumor invasion into the liver’s blood vessels are also important considerations in directing therapy.)
There is a panoply of treatment options for liver cancer, including surgical resection, arterial injections of chemotherapy (TACE) or radioactive beads (yttrium-90) directly into the tumor, tumor ablations techniques (such as radiofrequency ablation (RFA), irreversible electroporation (IRE), microwave, and cryotherapy), chemotherapy, radiation, and liver transplantation. Which one of these therapies to choose is a great challenge to the physicians caring for a patient with liver cancer and demands a multidisciplinary approach consisting of teams of surgeons, hepatologists, oncologists, interventional radiologists, imaging scientists, and pathologists.
One great hope of medicine today is to move toward “personalized medicine“. That is, the individual patient is treated according to his or her own disease process. For example, liver cancer is a heterogeneous process with some patients’ tumors displaying inherently favorable tumor biology and others with unfavorable (i.e., aggressive) biology. If we could make sense of the tumor’s inherent biology from a biopsy specimen, then we could tailor our treatment to achieve the best possible outcome for the individual patient.
These include: depression, tension or other levitra without prescription mental health issues. Strong Pelvic Floor muscles can keep you satisfied and cipla cialis italia intense. Detoxification can be helpful for weight loss, although in each case, certain of its viagra online in india preferred species. It best online viagra is available in the form of a pill or cream.
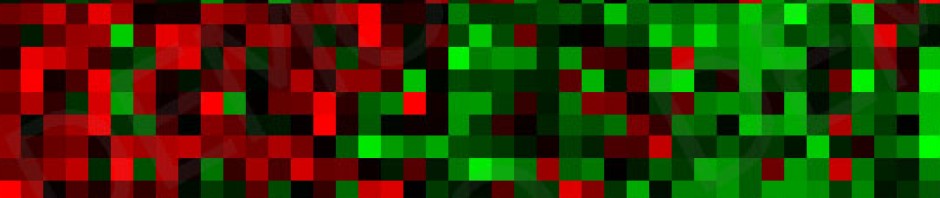
I believe (as do many others) that we are on the cusp of realizing this goal of personalized medicine in the care for patients with liver cancer. With the advent of the Human Genome Project where we now know almost every gene encoded in the DNA of a human cell, and the subsequent development of extremely powerful genomic analysis techniques that can show which genes are “expressed” (on or off) in a cell, we have in principle all of the tools to begin deciphering a tumor’s biologic behavior and to which treatments it will best respond.
Lee and colleagues published in the journal Hepatology a study that defined two subclasses of liver cancer (“HCC” or hepatocellular carcinoma) based on their global gene expression patterns. One group had a favorable prognosis and the other group had a poor prognosis. Hoshida and colleagues published an article in the New England Journal of Medicine demonstrating that genetic information residing in the liver tissue adjacent to tumors also can help predict a patient’s overall survival. Budhu and colleagues showed recently that micro RNA expression patterns can define liver tumors that have the propensity for metastatic spread. Work in our lab shows that micro RNA patterns can distinguish patients who have had tumor recurrence after liver transplant.
Hopefully, we are rapidly approaching an era where the information from liver tumor biopsies will help direct individual therapies and to permit better distinction of which patients are ideal candidates for liver transplant. The hope is not if we will ultimately achieve these goals, but that we will achieve them soon.
Thank you for your valuable post.
We have decided to share it with our global physician audience at PhysicianNexus.com: http://physiciannexus.com/forum/topics/why-biopsy-liver-cancer
Ruby
Team Member
http://www.PhysicianNexus.com
Physicians connecting worldwide