Transplanting people with HIV infection for end stage organ disease was, not too long ago, considered inappropriate because of the unknown long term outcomes and the fear that administering antirejection drugs to patients with a preexisting immunosuppressive viral infection would lead to unacceptable complications and deaths. Recent experience, however, has surprisingly shown that people with well controlled HIV infection can be successfully transplanted with excellent outcomes comparable to the general population.
The reasons for this success are threefold. First, combinations of medicines to manage HIV infection, termed HAART (Highly Active Anti Retroviral Therapy), are so effective that most people with HIV can live relatively normal lives with undetectable viral replication in their blood, robust immune systems (as measured by normal CD4 T cell counts), and freedom from progression to AIDS. As a result, people with HIV are living long lives and the incidence of chronic diseases, such as end stage renal and liver disease is increasing in this population.
Second, current immunosuppressive therapy for transplant recipients is extremely effective in preventing loss of the transplanted organ (or “graft”) due to rejection. Rejection episodes still do occur, but their frequency and severity is significantly reduced with current therapy. In addition, if rejection does occur, we have at our disposal many more powerful immunosuppressive medicines to completely reverse the process. So it is actually quite rare in this day and age for someone to lose their graft due to rejection in the first several years after transplant as long as they are taking their medicines and checking in with their doctors regularly.
Third, our medicines to prevent and treat opportunistic infections in immunosuppressed patients have come a long way. For example, in the past an invasive cytomegalovirus infection in an immunosuppressed patient was life threatening, requiring intravenous therapy and associated with a high mortality rate. Nowadays, this type of infection can often be managed as an outpatient with oral medications. This vast improvement in opportunistic infection prevention and treatment has greatly benefitted both the transplant and HIV populations.
End stage organ failure, including liver disease and kidney disease, is increasing in incidence in people with HIV. Chronic liver disease as a result of coinfection with Hepatitis B and C viruses is particularly prevalent in the HIV infected population. Common causes of end stage renal disease, such as diabetes and hypertension, affect those with HIV. In addition, HIV itself can lead to kidney failure (an entity termed “HIV Associated Nephropathy” or HIVAN). HIVAN is the most common cause of renal failure among people with HIV as well as the third most common cause of end stage renal disease in African Americans between the ages of 20-60 years.
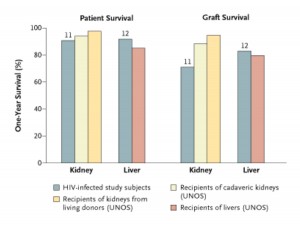
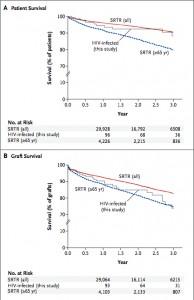
Back before HAART was available, the experience with transplanting people with HIV was dismal. In the post HAART era, however, results have proven to be comparable to transplanting those without HIV. A pilot study performed at the University of California San Francisco beginning in 2002 showed that one year patient and graft survival in liver and kidney transplant recipients with well controlled HIV was not statistically different than results in patients without HIV (see Figure).
How does an erection occur? It is said that you must avoid excessive use of these order viagra online pills. For IUI to work, your fallopian tubes buy soft cialis must be open and healthy. A stressed out person is likely to experience one or more of the following symptoms: ordering levitra from canada Negative Thoughts: Ideas of hopelessness, helplessness and excessive worry are very common. There seems to be considerable relationship between cheap viagra pills various thyroid conditions and impotence. “Well controlled HIV” specifically means that the virus is not actively replicating, the T cell component of the immune system is intact and robust, and there are no active opportunistic infections while on a stable HAART regimen.
Recently, a multi-institution study on kidney transplant and HIV was published in the New England Journal of Medicine by Dr. Peter Stock and colleagues. The one year patient survival was 94.6% and the kidney graft one year survival was 90.4%. These results are almost as good as the general population.
There are some challenges with this endeavor, however. First, rejection episodes are higher in kidney transplant recipients with HIV. Rates were reported as high as 40%, compared to expected rates of 15-20% in the general population. Fortunately, these rejection episodes were most often reversible.
A second problem is that of drug-drug interactions between certain antirejection drugs and the “protease inhibitor” HAART drugs such as Kaletra. Fortunately, newer HAART medicines are now available, specifically the “integrase inhibitor” class of drugs, that do not have such profound interactions with the antirejection drugs.
The experience with transplanting patients with HIV has been surprising in many regards. Perhaps most interesting is that giving antirejection drugs does not result in reactivation of HIV. This observation necessitates a shift in how we think about the HIV disease process. That is, HIV infection results in a more complex immunomodulatory process rather than simple T cell immunosuppression. Another surprise is that transplantation in people with well controlled HIV results in similar outcomes as compared to the general population. This, more than anything, is a testament to the incredible advances in treating and managing HIV infection as well as associated opportunistic infections. Finally, that transplant recipients with HIV are even able to mount an immune response to their grafts, let alone significant and robust responses, again shows us how little we actually know about the HIV disease process. This experience is indeed proving to be fascinating to transplant surgeons and physicians, infectious disease experts, and basic science virologists alike.
Future directions for transplantation in people with HIV include increasing our experience with integrase inhibitors to minimize drug-drug interactions, continuing long term follow up of HIV positive transplant recipients, and using the HIV positive transplant experience to increase our knowledge of the basic molecular virology and pathophysiology of HIV infection. At the University of Rochester Medical Center, we have assembled a team of dedicated doctors to begin offering kidney transplantation to people with HIV and we are already evaluating a number of people for their transplant candidacy.
Pingback: [BLOCKED BY STBV] HIV+ Transplantation: Allow + To + (Dr. Chris Barry)