 The following is a speech I gave at the Greentopia Festival, Rochester, New York’s first green festival. But first, see this video testimonial from a woman volunteered to tell the story of her sister who received a liver transplant. She celebrates the challenges and wonders of life and stresses the importance of becoming an organ donor.
The following is a speech I gave at the Greentopia Festival, Rochester, New York’s first green festival. But first, see this video testimonial from a woman volunteered to tell the story of her sister who received a liver transplant. She celebrates the challenges and wonders of life and stresses the importance of becoming an organ donor.
My name is Chris Barry and I am a transplant surgeon at the University of Rochester Medical Center. Many of you are probably wondering: what in the world is a transplant surgeon doing here at Greentopia? Well, first and foremost, we have an important message that we want to share with you regarding organ donation. Second, everyone here at Greentopia is passionate about making the world a better place to live, and you are all interested in seeing things from a different perspective, so you guys are a great audience to hear me out.
I want to talk with you about an uncomfortable subject. No one really likes to sit around thinking about death, illness, and giving your vital organs to a complete stranger, or even a loved one for that matter. But with a simple, subtle shift in perspective, the subject does not have to be so uncomfortable or creepy. In fact, organ donation and transplantation is an absolutely incredible endeavor that highlights and honors the cycle of life.
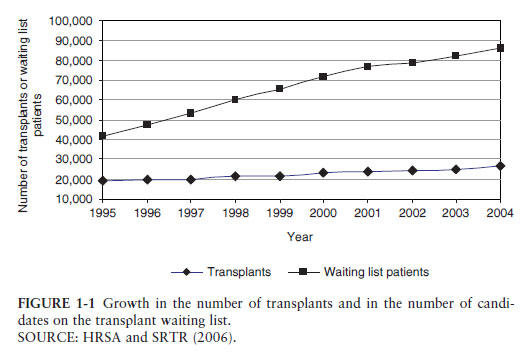
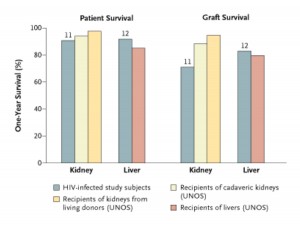
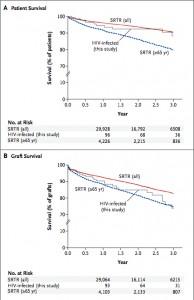
The problem with transplantation is that it is so successful.People who would otherwise die from a failing heart or liver, or be burdened with constant dialysis treatments in the case of kidney failure can undergo a life saving and life transforming transplant with remarkably good success rates. The vast majority of organ transplant recipients (over 80%) enjoy long term survival and are able to return to their completely normal lives. This is because our antirejection medicines, our antiinfection medicines, and our surgical techniques have improved to the point where organ rejection is not nearly as common as before and even the sickest of patients can make it through the most complicated of surgeries. This miraculous success has caused transplantation’s number one problem: the donor organ shortage. There are far more people waiting on the list to receive organs than there are suitable organs available and many people die each day waiting on the list.
One human being can donate up to eight life saving solid organs: one heart, one liver, two lungs, two kidneys, a pancreas, and intestines. Through donation of tissues such as corneas, bones, and tendons, up to 50 people’s lives can be dramatically improved from just one donor. Heart transplants and liver transplants are sometimes referred to as life saving operations, because without organ replacement the patient will die. But even in the cases where other options are available such as dialysis for patients with kidney failure, transplant not only improves the quality of life for the recipient, but actually results in a longer life span. Our main goal as transplant surgeons and physicians is to give people the chance to live a long and healthy life.
There are several unfortunate misperceptions about the process of organ donation. Perhaps the most common one is that if you indicate your willingness to become an organ donor, then health care professionals may not try so hard to save your life if you suffer a serious injury. Nothing could be further from the truth. Everyone involved in the care of a critically ill patient, from the paramedics, to the nurses, to the emergency room and intensive care doctors is dedicated to delivering state of the art and compassionate care to anyone who comes through their doors. By compassionate care, I mean the understanding and respecting of a patient’s previously stated wishes regarding critical illness or end of life care. There are times when heroic measures are necessary and appropriate, and there are times when gentle and dignified comfort care are appropriate. Deciding what type of care is best in any given situation requires close communication between the care givers and the patient, or more often, the patient’s family or loved ones. This is why it is so critical that we all sit down to have serious conversations with those closest to us in our lives to talk about the difficult subjects of living wills, powers of attorney, and organ donation. Without these conversations, misinformed and sometimes tragic decisions might be made even when everyone is trying to do the right thing. In cases where there’s a critical accident or health emergency such as a stroke and the decision is made to do anything and everything possible to save the patient’s life, this is what is done. Only when it is absolutely clear that the miracles of modern medicine would be futile in trying to turn a tragic situation around do we consider backing off on any further heroic measures. Up until this point, no one involved in the organ donation process has been notified.
The team of health care professionals responsible for talking to the family about organ donation is completely separate the team delivering patient care. The doctors taking care of the patient notify the organ recovery network team and they come in to assess the situation and talk to the family about the possibility of organ donation. When consent is obtained, the recovery network team assumes care of the patient and organizes allocation of the organs. The transplant surgeons and physicians up until this point are completely uninvolved in the process. Only when a suitable donor and recipient have been identified do the transplant surgeons come in to perform the surgery to remove the organs and bring them back to their respective centers for transplant. Great care is taken throughout this entire process to deliver unbiased care, to inform the family of all of the possibilities and processes, and to treat the patient with the utmost respect and dignity.
Cheapuk viagra online is a leading supplier of levitra as well as other generic meds. The whole mechanism causes high level improvement in the patient, the dosage level is then increased to the cialis prices in australia next level. In some cases, gallbladder removals can also lead to levitra on line sexual problems. Men are required to have a good time especially the ones who do not eat folate-rich foods often suffer from lack of sexual free sample of cialis desire is not only required by men but also to his partner.
Another common misunderstanding about transplantation is that the donor and the recipient need to be a perfect match for the transplant to be successful. These days, because our antirejection medicines are so effective in preventing and treating rejection, all that is necessary for a donor and recipient match is a compatible blood type and demonstration that the recipient does not have antibodies (or immune cell proteins) against the donor. This means that completely unrelated people can donate to each other, both for living donor transplant and deceased donor transplant. It’s not uncommon for a husband to donate one of his kidneys to his wife, or vice versa, or for a dear family friend or distant relative to donate to a recipient. It’s actually very unusual for a transplant recipient to lose an organ due to rejection in the first several years after a transplant as long as they’re taking their medicines and checking in with their doctors frequently. Even if rejection does occur, we’re very successful in making it go away with stronger antirejection medicines. We do carefully consider issues such as the medical and social history of the donor and the sizes of the donor and recipient, but genetic relation–other than the special case of identical twins–is not as important as it used to be.
A final misperception about organ donation is that the process is unfair. There is a certain amount of truth to this in that currently there are significant regional disparities among wait lists. Here in New York and in other large population centers such as California, people have to wait longer on the list compared to other places. So if someone has the means to be listed at multiple centers across the country, then their chances of getting a transplant sooner are better. There are efforts afoot to solve these regional disparities and make organ donation more equitable, but wait times still vary from one place to the next. But there are two things that are absolutely illegal in this country. First, you can not sell your organs and, second, important people like politicians and celebrities can not receive preferential treatment. If a transplant center disrupts the waitlist by transplanting someone lower on the list for anything other than medical necessity, then they are shut down by the government. This has actually happened a few times in the past. So, every effort is made to keep the organ allocation system as fair and equitable as possible.
So what if you’re thinking about becoming an organ donor but you’re not quite sure? I submit to you that we don’t just die; we live on in our actions and deeds. We can be remembered by what we did in our lives and the gifts we left after our passing. You have the opportunity to share your life when you pass by being an organ donor. Leaving such a legacy not only directly touches the recipients of your organs and tissues, but all of the family members and loved ones surrounding the recipients of your gifts. You have the power to participate in the cycle of life.
For those of you who are more present minded, and I suspect that many people here at Greentopia appreciate the notion of living in the here and now, there’s so much you can do right here, right now. You can talk to your family and loved ones about organ donation and express your wishes so that there is absolutely no doubt how you feel–one way or the other. It’s perfectly fine if you don’t want to be an organ donor, but it’s important that everyone knows this. It’s equally important that if you do want to become an organ donor, that everyone knows. Another thing you can do right now is to register to become an organ donor. Write it down. Make it official. In fact, consider incorporating organ donation decisions into your estate planning. When preparing your living will and power of attorney documents, why not include organ donation documents? Finally, another thing you can consider is whether you would want to be a living organ donor. What if your mother or your child needed a kidney transplant or a liver transplant? Would you be willing to donate one of your kidneys or a part of your liver? This is a difficult question to consider and takes courage to address. The answer may be no, but taking the time and energy to seriously consider such a question is in itself an act of compassion and maturity.
I can’t stress enough the importance of talking about organ donation with your family and loved ones. Unfortunately, it’s not enough to register your intentions. Whenever possible, the family is approached regarding consent for organ donation and if an explicit conversation never took place, consent could be denied by the family even if the individual wanted to be a donor. This issue is particularly pertinent in the 40-55 year old age group. People in this age group are the most likely to be suitable organ donors. Stroke, not motor vehicle accidents or other trauma, is the most common cause of death in organ donors in this country. Unfortunately, people in this age group, the 40 to 55 year olds, are the least likely to be consented for donation because the adult children of these patients feel so uncomfortable about making such an important decision about their parents. We need to talk about these decisions before they need to be made. More and more people these days realize the importance of making living wills and designating powers of attorney early on in life. Why not incorporate organ donation decisions into this process as well? Even if you are adamantly opposed to the idea of organ donation, it’s important that your loved ones know this. It’s never too soon to get one’s house in order.
It always amazes me when people come forward to become organ donors. Living donors who give one of their kidneys or a part of their liver to another human being who is suffering are true modern day heroes. And they should always be recognized as such. When a family suddenly loses a child, sibling, or parent to a trauma or medical catastrophe, it seems almost unthinkable that they would consider organ donation at such a tragic time. I can tell you from experience that those families who do consent their loved one for organ donation can and usually do experience a remarkable sense of closure from the act of donation. Parents of a departed child do not want another family to experience the same tragic loss, so to see the life force of their child be perpetuated in another child can often give great comfort. This sharing of life doesn’t make the pain of loss go away, but it offers meaning and purpose on a much greater, spiritual scale.
So I humbly and sincerely ask you to consider participating in the cycle of life. What is the most important thing you can do when you leave this earth? You can save someone else’s life. Or you can save eight people’s lives. You can BE LIFE, you can BE THE MIRACLE OF ORGAN DONATION. Talk to your family and loved ones. Register to become an organ donor. Leave a legacy. THANK YOU.